What is Whiplash ?
Whiplash is an injury to the neck and upper back that can occur following an auto accident. Whiplash can also occur in other circumstances where the neck is forced backwards and then forwards such as a fall or during a sporting event. In automobile accidents, whiplash occurs as a result of sudden "acceleration - deceleration" forced to the spine and soft tissue structures (tendons, ligaments and muscles):
Whiplash Associated Disorder (WAD), describes a more serious and chronic condition which can include symptoms other than just pain and stiffness in the neck such as: nausea, dizziness, headaches, ringing in the ears, concussion, etc.
In automobile accidents, the most common form of impact for whiplash is a rear end type of impact. There are many factors contributing to the injury including: speed of impact, type of seat, type of vehicle, did the occupant brace for impact ? was the occupant looking straight ahead or turned ? etc.
Whiplash can be quantified on X-ray as an "S-Shaped curve":
It has been well documented that soft tissue structures are injured and which are responsible for localized pain and stiffness. Pain and tingling down the arm(s) can be a sign of a more serious condition such as a cervical disc herniation or a brachial plexus lesion or compression.
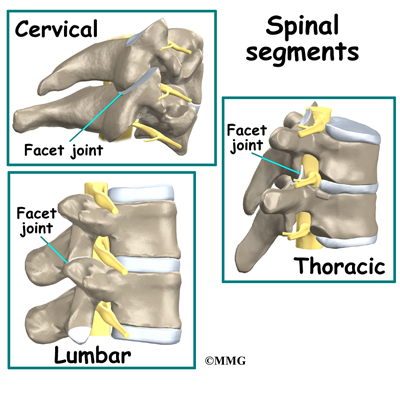
This recent study suggests what Chiropractors have always known, that there is injury to cervical zygapophysial joints OR facet joints following whiplash. Facet joints are located at each level of our vertebrae and are the joints responsible for the "popping or crackling sounds" that we hear from our spines. Facet joints are also the joints that are "adjusted" when Chiropractors manipulate the spine. Perhaps that is why so many patients have found relief with Chiropractic following an automobile accident causing whiplash.
Diagram showing Facet joints:
Have you been injured in an automobile accident and are suffering from whiplash, headaches or an injury to a spinal disc and nerve ? Call us at (650) 347-2225 to get a correct diagnosis and appropriate treatment. We offer treatment for soft tissue injuries, injuries to the facet joints and cervical disc's. Dr. Hindocha is a Chiropractor in San Mateo who has had over 10 years of experience managing these difficult cases. Moreover, Dr. Hindocha shares his office space with a Physical Medicine & Rehabilitation and Orthopedic specialist should you require advanced care. We offer: Chiropractic care, non-surgical spinal decompression therapy, PT modalities and procedures, therapeutic exercises such as cervical and lumbar core stabilization programs and traction procedures. We will work with your lawyer or can recommend an attorney qualified for your case. Dr. Hindocha's paperwork and medical reports can help support your case to avoid costly litigation.