From: J Manipulative Physiol Ther. 2010 Oct;33(8):576-84.
Spinal manipulation (sometimes referred to as a 'spinal adjustment') is the Chiropractors primary therapy. Microdiscectomy is a surgical procedure which removes a portion of the facet joint (part of the spine) as well as a portion of the herniated disc which is "pinching" the nerve root.
This study concluded: "Sixty percent of patients with sciatica who had failed other medical management benefited from spinal manipulation to the same degree as if they underwent surgical intervention. Of 40% left unsatisfied, subsequent surgical intervention confers excellent outcome. Patients with symptomatic LDH failing medical management should consider spinal manipulation followed by surgery if warranted."
Conclusions: Have sciatica ? Considering the surgical options ? Why not try Chiropractic Spinal Manipulation which, according to this study, has a 60% chance of giving you the same outcome as if you were to have surgery. If all else fails, the surgical option is always available right ? Well, why not try non-surgical VAX-D Spinal Decompression Therapy.
Dr. Hindocha performs Chiropractic therapy and non-surgical Spinal Decompression therapy in San Mateo, California. Have you been diagnosed with Sciatica, a Herniated, Bulging or "Slipped" disc ? Call Peninsula Spine & Sports Rehabilitation at (650) 347-2225 to find out if you can benefit with Chiropractic care or VAX-D Spinal Decompression therapy.
Friday, December 16, 2011
Do Chiropractic Physician services for the treatment of Low Back and Neck Pain improve the value of health benefit plans ?
Traditionally, Doctors and Insurance plans have often disagreed on how to manage a patients health. For a Doctor, we recommend treatments and diagnostic testing (X-ray, MRI, CT, nerve testing) which we feel will give us the most accurate diagnosis and therefore formulate a treatment plan tailored to our patients needs. Insurance plans see their clients as liabilities and have therefore have hired third party individuals specifically to deny care and therefore cut costs of medically necessary treatment and diagnostics.
The Foundation for Chiropractic progress funded the following study to determine the COST SAVINGS to health benefit plans utilizing Chiropractic care for neck and low back complaints compared to Physician visits:
In a 2009 study titled "Do Chiropractic Physician Services for Treatment of Low Back and Neck Pain Improve the Value of Health Benefit Plans ? An Evidence-Based Assessment of Incremental Impact on Population Health and Total Health Care Spending" by Niteesh Choudhry, MD, PhD from Harvard Medical School and Arnold Milstein, MD, MPH from Mercer Health and Benefits, San Francisco concluded:
"When considering the effectiveness and cost together, chiropractic physician care for low back and neck pain is highly cost effective, [and] represents good value in comparison to medical physician care and to widely accepted cost-effectiveness thresholds. Because we were unable to incorporate savings in drug spending commonly associated with US chiropractic care, our estimate of its comparitive cost effectiveness is likely understated."
What was compared was the costs associated with Chiropractic physician care for episodes of neck and low back pain vs. costs associated with traditional Medical care (Medical doctor visits, Hospital visits, outpatient Physical Therapy and interventions). Note: the costs associated with medications WERE NOT factored into the calculations therefore the estimate of its comparitive cost effectiveness is likely understated.
Dr. Rommel Hindocha is a practicing Chiropractor in San Mateo. We offer quality Chiropractic care for neck and low back conditions. We are participating providers on most medical insurance plans including PPO, HMO, Kaiser, Workers Compensation and accepting automobile insurance plans (Medical Payments). If you, or someone you know, has a neck or low back complaint, call Dr. Hindocha at Peninsula Spine and Sports Rehabilitation in San Mateo at (650) 347-2225.
Tuesday, November 29, 2011
Whiplash - Cervical Zygapophysial Joint Pain After Whiplash
From: On Cervical Zygapophysial Joint Pain After Whiplash. Bogduk, Nikolai MD, PhD. Spine: 1 December 2011 - Volume 36 - Issue - p S194–S199.
What is Whiplash ?
Whiplash is an injury to the neck and upper back that can occur following an auto accident. Whiplash can also occur in other circumstances where the neck is forced backwards and then forwards such as a fall or during a sporting event. In automobile accidents, whiplash occurs as a result of sudden "acceleration - deceleration" forced to the spine and soft tissue structures (tendons, ligaments and muscles):
Whiplash Associated Disorder (WAD), describes a more serious and chronic condition which can include symptoms other than just pain and stiffness in the neck such as: nausea, dizziness, headaches, ringing in the ears, concussion, etc.
In automobile accidents, the most common form of impact for whiplash is a rear end type of impact. There are many factors contributing to the injury including: speed of impact, type of seat, type of vehicle, did the occupant brace for impact ? was the occupant looking straight ahead or turned ? etc.
Whiplash can be quantified on X-ray as an "S-Shaped curve":
It has been well documented that soft tissue structures are injured and which are responsible for localized pain and stiffness. Pain and tingling down the arm(s) can be a sign of a more serious condition such as a cervical disc herniation or a brachial plexus lesion or compression.
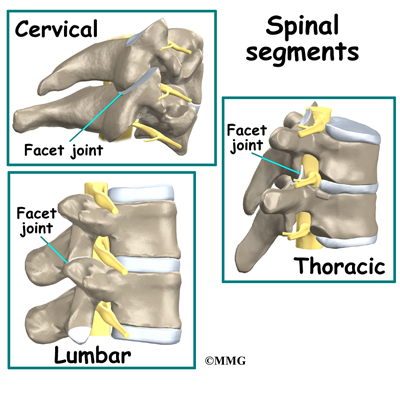
This recent study suggests what Chiropractors have always known, that there is injury to cervical zygapophysial joints OR facet joints following whiplash. Facet joints are located at each level of our vertebrae and are the joints responsible for the "popping or crackling sounds" that we hear from our spines. Facet joints are also the joints that are "adjusted" when Chiropractors manipulate the spine. Perhaps that is why so many patients have found relief with Chiropractic following an automobile accident causing whiplash.
Diagram showing Facet joints:
Have you been injured in an automobile accident and are suffering from whiplash, headaches or an injury to a spinal disc and nerve ? Call us at (650) 347-2225 to get a correct diagnosis and appropriate treatment. We offer treatment for soft tissue injuries, injuries to the facet joints and cervical disc's. Dr. Hindocha is a Chiropractor in San Mateo who has had over 10 years of experience managing these difficult cases. Moreover, Dr. Hindocha shares his office space with a Physical Medicine & Rehabilitation and Orthopedic specialist should you require advanced care. We offer: Chiropractic care, non-surgical spinal decompression therapy, PT modalities and procedures, therapeutic exercises such as cervical and lumbar core stabilization programs and traction procedures. We will work with your lawyer or can recommend an attorney qualified for your case. Dr. Hindocha's paperwork and medical reports can help support your case to avoid costly litigation.
What is Whiplash ?
Whiplash is an injury to the neck and upper back that can occur following an auto accident. Whiplash can also occur in other circumstances where the neck is forced backwards and then forwards such as a fall or during a sporting event. In automobile accidents, whiplash occurs as a result of sudden "acceleration - deceleration" forced to the spine and soft tissue structures (tendons, ligaments and muscles):
Whiplash Associated Disorder (WAD), describes a more serious and chronic condition which can include symptoms other than just pain and stiffness in the neck such as: nausea, dizziness, headaches, ringing in the ears, concussion, etc.
In automobile accidents, the most common form of impact for whiplash is a rear end type of impact. There are many factors contributing to the injury including: speed of impact, type of seat, type of vehicle, did the occupant brace for impact ? was the occupant looking straight ahead or turned ? etc.
Whiplash can be quantified on X-ray as an "S-Shaped curve":
It has been well documented that soft tissue structures are injured and which are responsible for localized pain and stiffness. Pain and tingling down the arm(s) can be a sign of a more serious condition such as a cervical disc herniation or a brachial plexus lesion or compression.
This recent study suggests what Chiropractors have always known, that there is injury to cervical zygapophysial joints OR facet joints following whiplash. Facet joints are located at each level of our vertebrae and are the joints responsible for the "popping or crackling sounds" that we hear from our spines. Facet joints are also the joints that are "adjusted" when Chiropractors manipulate the spine. Perhaps that is why so many patients have found relief with Chiropractic following an automobile accident causing whiplash.
Diagram showing Facet joints:
Have you been injured in an automobile accident and are suffering from whiplash, headaches or an injury to a spinal disc and nerve ? Call us at (650) 347-2225 to get a correct diagnosis and appropriate treatment. We offer treatment for soft tissue injuries, injuries to the facet joints and cervical disc's. Dr. Hindocha is a Chiropractor in San Mateo who has had over 10 years of experience managing these difficult cases. Moreover, Dr. Hindocha shares his office space with a Physical Medicine & Rehabilitation and Orthopedic specialist should you require advanced care. We offer: Chiropractic care, non-surgical spinal decompression therapy, PT modalities and procedures, therapeutic exercises such as cervical and lumbar core stabilization programs and traction procedures. We will work with your lawyer or can recommend an attorney qualified for your case. Dr. Hindocha's paperwork and medical reports can help support your case to avoid costly litigation.
Assessing the outcomes after Spinal Fusion surgery.
From: Perioperative Morbidity and Mortality After Anterior, Posterior, and Anterior/Posterior Spine Fusion Surgery. Stavros G. Memtsoudis, MD, PhD; Vassilios I. Vougioukas, MD, PhD; Yan Ma, PhD; Licia K. Gaber-Baylis, BA; Federico P. Girardi, MD. Spine. 2011;36(22):1867-1877. © 2011 Lippincott Williams & Wilkins.
The utilization of Spinal fusion techniques have increased dramatically despite the relatively few studies showing the safety of this procedure. There is also a relative lack of studies comparing the relative spinal surgical techniques and the outcomes associated with them.
This study was designed to assess the Morbidity (the rate of incidence) and Mortality (the measure of the number of deaths) and to determine the independent risk factors for in-hospital death. associated with the various surgical approaches to spinal fusion surgery.
The outcomes being measured were: Perioperative (after operation) of Anterior Spinal Fusion (ASF), Posterior Spinal Fusion (PSF) and APSF (Anterior Posterior Spinal Fusion).
Here are some X-rays, post-operative:
Results of the study:
There was an increased incidence of perioperative complications and adjusted risk of in-hospital mortality among hospital admissions undergoing APSF and ASF when compared to PSF procedures.
The highest rates of fatal outcomes and complications were associated with procedures using the anterior thoracic approach.
Risk factors for in-hospital mortality included the following: male gender, advanced age, procedures indicated for metastatic disease and trauma, as well as the presence of several comorbidities and perioperative complications.
Procedures involving the anterior spine were associated with higher morbidity and mortality in our study, despite being performed in younger individuals with lower comorbidity burden.
The highest rate of morbidity and mortality was seen in APSF patients, which can be explained by longer surgical times, more blood loss, and increased surgical complexity.
When studying patient demographics and their association with mortality, we found increased independent risk of a fatal event after spine fusion among men.
We identified an increased incidence of morbidity and risk for mortality in patients with advanced age. Patients over the age of 75 years made up almost one- third of all mortalities, despite representing less than 9% of the spine surgical population in this study.
Pulmonary circulatory disease, congestive heart failure, renal disease, and coagulopathies were associated with the highest increases of risk for perioperative mortality.
Perioperative complications were also associated with increases in the odds of a fatal event. Pulmonary embolism, perioperative shock, ARDS, and cardiac complications were associated with the highest risk of mortality. All of these events had the highest incidence among APSF patients.
It was determined that APSF and ASF carried an increased adjusted risk of in-hospital mortality and greater incidence of in-hospital complications when compared to PSF procedures.
What can we learn from this study ? Like the old saying goes "an ounce of prevention equals a pound of cure". Aside from unforeseen circumstances such as trauma, there are ways we can help prevent our spines from getting to this level of degeneration.
1.) Have a spinal exam and check up.
2.) Don't ignore early signs such as: recurring back pain that may self-resolve or resolve with medications. In my experience, most cases of spinal degeneration and herniated discs have manifested themselves in the past and have not been adequately or properly treated. Chiropractic therapy is a drugless, non-surgical, intervention which can help with many types of back pain.
3.) For those of you who have already reached the advanced stages of spinal arthritis, osteroarthritis, degenerative disc disease, sciatica or have one or multiple herniated discs, VAX-D spinal decompression therapy is an alternative approach to some types of surgery and "endless" epidural injections.
4.) Exercise, lose weight and keep a healthy lifestyle.
Dr. Rommel Hindocha is a Chiropractor in San Mateo California. In addition to Chiropractic therapy, he does perform non-surgical Spinal Decompression therapy at 101 S. San Mateo Drive, Suite 200, San Mateo, CA 94401. You can reach Peninsula Spine & Sports Rehabilitation at (650) 347-2225.
The utilization of Spinal fusion techniques have increased dramatically despite the relatively few studies showing the safety of this procedure. There is also a relative lack of studies comparing the relative spinal surgical techniques and the outcomes associated with them.
This study was designed to assess the Morbidity (the rate of incidence) and Mortality (the measure of the number of deaths) and to determine the independent risk factors for in-hospital death. associated with the various surgical approaches to spinal fusion surgery.
The outcomes being measured were: Perioperative (after operation) of Anterior Spinal Fusion (ASF), Posterior Spinal Fusion (PSF) and APSF (Anterior Posterior Spinal Fusion).
Here are some X-rays, post-operative:
Results of the study:
There was an increased incidence of perioperative complications and adjusted risk of in-hospital mortality among hospital admissions undergoing APSF and ASF when compared to PSF procedures.
The highest rates of fatal outcomes and complications were associated with procedures using the anterior thoracic approach.
Risk factors for in-hospital mortality included the following: male gender, advanced age, procedures indicated for metastatic disease and trauma, as well as the presence of several comorbidities and perioperative complications.
Procedures involving the anterior spine were associated with higher morbidity and mortality in our study, despite being performed in younger individuals with lower comorbidity burden.
The highest rate of morbidity and mortality was seen in APSF patients, which can be explained by longer surgical times, more blood loss, and increased surgical complexity.
When studying patient demographics and their association with mortality, we found increased independent risk of a fatal event after spine fusion among men.
We identified an increased incidence of morbidity and risk for mortality in patients with advanced age. Patients over the age of 75 years made up almost one- third of all mortalities, despite representing less than 9% of the spine surgical population in this study.
Pulmonary circulatory disease, congestive heart failure, renal disease, and coagulopathies were associated with the highest increases of risk for perioperative mortality.
Perioperative complications were also associated with increases in the odds of a fatal event. Pulmonary embolism, perioperative shock, ARDS, and cardiac complications were associated with the highest risk of mortality. All of these events had the highest incidence among APSF patients.
It was determined that APSF and ASF carried an increased adjusted risk of in-hospital mortality and greater incidence of in-hospital complications when compared to PSF procedures.
What can we learn from this study ? Like the old saying goes "an ounce of prevention equals a pound of cure". Aside from unforeseen circumstances such as trauma, there are ways we can help prevent our spines from getting to this level of degeneration.
1.) Have a spinal exam and check up.
2.) Don't ignore early signs such as: recurring back pain that may self-resolve or resolve with medications. In my experience, most cases of spinal degeneration and herniated discs have manifested themselves in the past and have not been adequately or properly treated. Chiropractic therapy is a drugless, non-surgical, intervention which can help with many types of back pain.
3.) For those of you who have already reached the advanced stages of spinal arthritis, osteroarthritis, degenerative disc disease, sciatica or have one or multiple herniated discs, VAX-D spinal decompression therapy is an alternative approach to some types of surgery and "endless" epidural injections.
4.) Exercise, lose weight and keep a healthy lifestyle.
Dr. Rommel Hindocha is a Chiropractor in San Mateo California. In addition to Chiropractic therapy, he does perform non-surgical Spinal Decompression therapy at 101 S. San Mateo Drive, Suite 200, San Mateo, CA 94401. You can reach Peninsula Spine & Sports Rehabilitation at (650) 347-2225.
Wednesday, November 2, 2011
Is there a genetic predisposition to "Back Disease" ?
J Bone Joint Surg Am. 2011;93:225-229. Abstract
In an analysis of a database of more than 2 million people, first-degree and third-degree relatives of people with lumbar disc disease had a significantly increased relative risk of developing the back condition themselves compared with expected rates for the general population. "The results of this study support a heritable predisposition to lumbar disc disease," lead author Alpesh A. Patel, MD, and colleagues from the departments of Orthopaedics and Biomedical Informatics, University of Utah School of Medicine, Salt Lake City, report in the February 2 issue of the Journal of Bone and Joint Surgery.
To test the hypothesis that lumbar disc disease may be inherited, the authors analyzed data from both the Utah Population Database, which permits the tracking of medical information on the founding pioneers of Utah and their descendents, and the University of Utah Health Sciences Center data warehouse, which has diagnosis and procedure data on all patients treated at the University Hospital. Together, the databases contain information on more than 2.4 million patients. Only patients and control participants with at least 3 generations of genealogical data were included in the study.
Of those individuals, 1254 people had at least 1 diagnosis of lumbar disc disease or lumbar disc herniation, along with the requisite genealogical data. The authors tested for heritability in 2 ways: by estimating the relative risk for lumbar disease in relatives and by determining a genealogical index of familiality (GIF). They compared their findings in affected families with the expected results for the general population of Utah.
First-degree relatives of people with lumbar disc disease had a relative risk of 4.15 of having the disease themselves (95% confidence interval [CI], 2.82 - 6.10; P < .001). In third-degree relatives, the relative risk was 1.46 (95% CI, 1.06 - 2.01; P = .027). Relative risk was slightly elevated in second-degree relatives, at 1.15, but this was not significant (95% CI, .71 - 1.87; P = .60), perhaps because of limitations in the data.
Conclusions:
This study suggests that first-degree relatives and third degree relatives have a statistically significant of developing lumbar disc disease and that there may be a genetic component related to disc disease.
Future research can potentially identify the genes leading lumbar disc disease which often accompanies lumbar disc herniations and spinal arthritis.
Chiropractic spinal manipulation has been thought to restore motion to individual spinal segments, thus increasing range of motion and equalizing the bio mechanical loads on the spinal structures. In cases of Sciatica, Disc Herniations and advanced Spinal Arthritis and Lumbar Disc Disease, VAX-D Spinal Decompression Therapy is a relatively new therapy which has shown good results in relieving pain, reduce the size of the disc herniations and increasing functional and overall quality of life for those suffering from these conditions.
Dr. Hindocha, at Peninsula Spine & Sports Rehabilitation in San Mateo, offers gentle Chiropractic therapy and non-surgical Spinal Decompression Therapy. Dr. Hindocha offers Chiropractic therapy in his San Mateo and San Francisco locations and VAX-D Spinal Decompression Therapy in San Mateo. Please call us at (650) 347-2225 to see if you are a candidate and schedule your consultation.
In an analysis of a database of more than 2 million people, first-degree and third-degree relatives of people with lumbar disc disease had a significantly increased relative risk of developing the back condition themselves compared with expected rates for the general population. "The results of this study support a heritable predisposition to lumbar disc disease," lead author Alpesh A. Patel, MD, and colleagues from the departments of Orthopaedics and Biomedical Informatics, University of Utah School of Medicine, Salt Lake City, report in the February 2 issue of the Journal of Bone and Joint Surgery.
To test the hypothesis that lumbar disc disease may be inherited, the authors analyzed data from both the Utah Population Database, which permits the tracking of medical information on the founding pioneers of Utah and their descendents, and the University of Utah Health Sciences Center data warehouse, which has diagnosis and procedure data on all patients treated at the University Hospital. Together, the databases contain information on more than 2.4 million patients. Only patients and control participants with at least 3 generations of genealogical data were included in the study.
Of those individuals, 1254 people had at least 1 diagnosis of lumbar disc disease or lumbar disc herniation, along with the requisite genealogical data. The authors tested for heritability in 2 ways: by estimating the relative risk for lumbar disease in relatives and by determining a genealogical index of familiality (GIF). They compared their findings in affected families with the expected results for the general population of Utah.
First-degree relatives of people with lumbar disc disease had a relative risk of 4.15 of having the disease themselves (95% confidence interval [CI], 2.82 - 6.10; P < .001). In third-degree relatives, the relative risk was 1.46 (95% CI, 1.06 - 2.01; P = .027). Relative risk was slightly elevated in second-degree relatives, at 1.15, but this was not significant (95% CI, .71 - 1.87; P = .60), perhaps because of limitations in the data.
Conclusions:
This study suggests that first-degree relatives and third degree relatives have a statistically significant of developing lumbar disc disease and that there may be a genetic component related to disc disease.
Future research can potentially identify the genes leading lumbar disc disease which often accompanies lumbar disc herniations and spinal arthritis.
Chiropractic spinal manipulation has been thought to restore motion to individual spinal segments, thus increasing range of motion and equalizing the bio mechanical loads on the spinal structures. In cases of Sciatica, Disc Herniations and advanced Spinal Arthritis and Lumbar Disc Disease, VAX-D Spinal Decompression Therapy is a relatively new therapy which has shown good results in relieving pain, reduce the size of the disc herniations and increasing functional and overall quality of life for those suffering from these conditions.
Dr. Hindocha, at Peninsula Spine & Sports Rehabilitation in San Mateo, offers gentle Chiropractic therapy and non-surgical Spinal Decompression Therapy. Dr. Hindocha offers Chiropractic therapy in his San Mateo and San Francisco locations and VAX-D Spinal Decompression Therapy in San Mateo. Please call us at (650) 347-2225 to see if you are a candidate and schedule your consultation.
Low Back Pain in Adolecents and Teens - Imaging
From: American Academy of Pediatrics (AAP) 2011 National Conference and Exhibition; Abstract #14782. Presented October 14, 2011.
No Imaging Needed for Most Low Back Pain in Teens
Low back pain is common in adolescents and teens. Most cases of low back pain are diagnosed as "mechanical low back pain", which is a diagnosis of "exclusion", ruling out any serious pathologies.
Mechanical low back pain is common in the pediatric population, and recent studies have shown that undiagnosable mechanical low back pain accounts for up to 78% of cases in adolescents. The most common pathologic cause of back pain in this age group is spondylolysis and spondylolisthesis
Most cases of low back pain in children will get better with conservative management, such as Chiropractic and do not need to be diagnosed with radiographic studies, researchers said here at the American Academy of Pediatrics (AAP) 2011 National Conference and Exhibition.
Parents often worry as low back pain can appear to be very serious at it's initial onset. However, the routine use of X-rays, CT scans and bone scans can complicated matters as it can expose your child to relatively high doses of radiation.
This study followed 2846 children aged 10 to 19 years who were seen at their institution with low back pain between 2000 and 2008. Most (63%) were female, and the average age was 14 years.
In 79% of the patients (n = 2244), the cause of their low back pain went undiagnosed. Spondylolysis, which was diagnosed in 272 patients (9.6%), was found by plain radiography in 234 patients (86%), by bone scanning in 34 patients (12.5%), and by computed tomography (CT) in 4 patients (1.5%).
Dr. Dennis Drummond, MD, who headed the stated concluded: "Our message is try and treat the low back pain conservatively. If they are 50% to 60% improved when you see them in 6 weeks, you’re probably on the right track. If the pain is all gone at 3 months, get them ready to go back to sports or usual activities. If there is just as much pain at 6 weeks, go back to the old system of more investigation, but the majority will get better by then."
At Peninsula Spine & Sports Rehabilitation in San Mateo, Dr. Hindocha treats Pediatric patients with gentle Chiropractic therapy, soft tissue procedures and therapeutic exercises for rehabilitation. Dr. Hindocha does not routinely prescribe the use of X-rays on his patients, Pediatric or Adult, but does so when there is a need or clinical justification for use of these procedures. If your child has low back pain, please call us at (650) 347-2225 to schedule a consultation.
No Imaging Needed for Most Low Back Pain in Teens
Low back pain is common in adolescents and teens. Most cases of low back pain are diagnosed as "mechanical low back pain", which is a diagnosis of "exclusion", ruling out any serious pathologies.
Mechanical low back pain is common in the pediatric population, and recent studies have shown that undiagnosable mechanical low back pain accounts for up to 78% of cases in adolescents. The most common pathologic cause of back pain in this age group is spondylolysis and spondylolisthesis
Most cases of low back pain in children will get better with conservative management, such as Chiropractic and do not need to be diagnosed with radiographic studies, researchers said here at the American Academy of Pediatrics (AAP) 2011 National Conference and Exhibition.
Parents often worry as low back pain can appear to be very serious at it's initial onset. However, the routine use of X-rays, CT scans and bone scans can complicated matters as it can expose your child to relatively high doses of radiation.
This study followed 2846 children aged 10 to 19 years who were seen at their institution with low back pain between 2000 and 2008. Most (63%) were female, and the average age was 14 years.
In 79% of the patients (n = 2244), the cause of their low back pain went undiagnosed. Spondylolysis, which was diagnosed in 272 patients (9.6%), was found by plain radiography in 234 patients (86%), by bone scanning in 34 patients (12.5%), and by computed tomography (CT) in 4 patients (1.5%).
Dr. Dennis Drummond, MD, who headed the stated concluded: "Our message is try and treat the low back pain conservatively. If they are 50% to 60% improved when you see them in 6 weeks, you’re probably on the right track. If the pain is all gone at 3 months, get them ready to go back to sports or usual activities. If there is just as much pain at 6 weeks, go back to the old system of more investigation, but the majority will get better by then."
At Peninsula Spine & Sports Rehabilitation in San Mateo, Dr. Hindocha treats Pediatric patients with gentle Chiropractic therapy, soft tissue procedures and therapeutic exercises for rehabilitation. Dr. Hindocha does not routinely prescribe the use of X-rays on his patients, Pediatric or Adult, but does so when there is a need or clinical justification for use of these procedures. If your child has low back pain, please call us at (650) 347-2225 to schedule a consultation.
Sunday, October 30, 2011
Diagnosis - Thoracic Outlet Syndrome
Thoracic Outlet Syndrome
Thoracic outlet syndrome is a type of Brachial Plexus lesion involving compression of the neural (nerves) and/or vascular (blood vessels) structures between the rib cage, collar bone and neck:
Compression can occur at 3 sites:
1.) At an abnormal cervical rib.
2.) At the clavicle (collar bone).
3.) At the anterior muscles of the neck called the Scalenes.
Symptoms:
Pain, numbness/tingling in the pinky and ring fingers (4th and 5th digits) and the inner forearm. Pain and tingling in the neck and shoulders areas which can be worsened by carrying something heavy. Poor circulation in the hand or forearm (a bluish color, cold hands, or a swollen arm.) Weakness of the muscles in the hand and arm.
Causes:
Sporting injuries, trauma such as Whiplash resulting from car or motorcycle accidents, poor posture, carrying heavy backpacks, birth trauma and other rare conditions such as tumors can cause Thoracic Outlet Syndrome.
Diagnosis:
Diagnosis of TOS is made by seeing a Doctor familiar with this condition which includes a thorough history, physical exam and Orthopedic and Neurologic tests and may include diagnostic tests such as: X-ray, MRI, CT angiogram and Electrodiagnostic evaluation (nerve tests).
Treatment:
In non-severe cases, most cases of Thoracic Outlet Syndrome can resolve without the need for surgical intervention. Chiropractic treatment includes: cervical spine and clavicle manipulation, soft tissue procedures such as transfriction massage or myofascial release, therapeutic exercises to stretch the scalene muscles and postural exercises.
At Peninsula Spine & Sports Rehabilitation in San Mateo, we offer a Chiropractic solution which is unique in that it addresses the osseous (bony) and soft tissue causes of Thoracic Outlet Syndrome. This condition is becoming increasingly prevalent due to poor posture associated with long term computer use. Call us at (650) 347-2225 for your initial consultation with Dr. Hindocha.
Thoracic outlet syndrome is a type of Brachial Plexus lesion involving compression of the neural (nerves) and/or vascular (blood vessels) structures between the rib cage, collar bone and neck:
Compression can occur at 3 sites:
1.) At an abnormal cervical rib.
2.) At the clavicle (collar bone).
3.) At the anterior muscles of the neck called the Scalenes.
Symptoms:
Pain, numbness/tingling in the pinky and ring fingers (4th and 5th digits) and the inner forearm. Pain and tingling in the neck and shoulders areas which can be worsened by carrying something heavy. Poor circulation in the hand or forearm (a bluish color, cold hands, or a swollen arm.) Weakness of the muscles in the hand and arm.
Causes:
Sporting injuries, trauma such as Whiplash resulting from car or motorcycle accidents, poor posture, carrying heavy backpacks, birth trauma and other rare conditions such as tumors can cause Thoracic Outlet Syndrome.
Diagnosis:
Diagnosis of TOS is made by seeing a Doctor familiar with this condition which includes a thorough history, physical exam and Orthopedic and Neurologic tests and may include diagnostic tests such as: X-ray, MRI, CT angiogram and Electrodiagnostic evaluation (nerve tests).
Treatment:
In non-severe cases, most cases of Thoracic Outlet Syndrome can resolve without the need for surgical intervention. Chiropractic treatment includes: cervical spine and clavicle manipulation, soft tissue procedures such as transfriction massage or myofascial release, therapeutic exercises to stretch the scalene muscles and postural exercises.
At Peninsula Spine & Sports Rehabilitation in San Mateo, we offer a Chiropractic solution which is unique in that it addresses the osseous (bony) and soft tissue causes of Thoracic Outlet Syndrome. This condition is becoming increasingly prevalent due to poor posture associated with long term computer use. Call us at (650) 347-2225 for your initial consultation with Dr. Hindocha.
Recovery of Brachial Plexus Lesions Resulting from Heavy Backpack use.
From: BMC Musculoskeletal Disorders. 2011;12(1) © 2011 BioMed Central, Ltd.
Brachial plexus lesions as a consequence of carrying a heavy backpack have been reported, but the typical clinical course and long-term consequences are not clear. Here we evaluated the clinical course and pattern of recovery of backpack palsy (BPP) in a large series of patients.
Eighty percent of the patients recovered totally within 9 months after the onset of weakness. Prolonged symptoms occurred in 15% of the patients, but daily activities were not affected. The weight of the carried load at the symptom onset significantly affected the severity of the muscle strength loss in the physiotherapeutic testing at the follow-up. The initial electromyography did not predict recovery. Genetic testing did not reveal de novo hereditary neuropathy with pressure palsies.
Conclusions: The prognosis of BPP is favorable in the vast majority of cases. Electromyography is useful for diagnosis. To prevent brachial plexus lesions, backpack loads greater than 40 kg should be avoided.
What is a Brachial Plexus injury ?
A brachial plexus injury is an injury to the the network of nerves that sends signals from your spine to your shoulder, arm and hand. A brachial plexus injury occurs when these nerves are stretched or, in the most serious cases, torn. This happens as result of your shoulder being pressed down forcefully while your head is pushed up and away from that shoulder.
Brachial Plexus injuries arise from: contact sports, poor posture, heavy backpack use (above), Whiplash injuries arising from auto or motorcycle accidents, infants can acquire this condition during birth and other rare occurrences such as tumors.
Most Brachial Plexus lesions are treated conservatively (with therapy and/or rest) but severe lesions require surgical intervention.
Brachial plexus lesions as a consequence of carrying a heavy backpack have been reported, but the typical clinical course and long-term consequences are not clear. Here we evaluated the clinical course and pattern of recovery of backpack palsy (BPP) in a large series of patients.
Eighty percent of the patients recovered totally within 9 months after the onset of weakness. Prolonged symptoms occurred in 15% of the patients, but daily activities were not affected. The weight of the carried load at the symptom onset significantly affected the severity of the muscle strength loss in the physiotherapeutic testing at the follow-up. The initial electromyography did not predict recovery. Genetic testing did not reveal de novo hereditary neuropathy with pressure palsies.
Conclusions: The prognosis of BPP is favorable in the vast majority of cases. Electromyography is useful for diagnosis. To prevent brachial plexus lesions, backpack loads greater than 40 kg should be avoided.
What is a Brachial Plexus injury ?
A brachial plexus injury is an injury to the the network of nerves that sends signals from your spine to your shoulder, arm and hand. A brachial plexus injury occurs when these nerves are stretched or, in the most serious cases, torn. This happens as result of your shoulder being pressed down forcefully while your head is pushed up and away from that shoulder.
Brachial Plexus injuries arise from: contact sports, poor posture, heavy backpack use (above), Whiplash injuries arising from auto or motorcycle accidents, infants can acquire this condition during birth and other rare occurrences such as tumors.
Most Brachial Plexus lesions are treated conservatively (with therapy and/or rest) but severe lesions require surgical intervention.
Symptoms:
Neck pain, burning, numbness/tingling and/or weakness into one or both arms.
One of the most common forms of Brachial Plexus lesions is a condition called Thoracic Outlet Syndrome which will be discussed in a separate post.
At Peninsula Spine & Sports Rehabilitation is San Mateo, Dr. Hindocha offers Chiropractic treatment of non-surgical Brachial Plexus lesions. Please call us at (650) 347-2225 for an initial consultation.
Saturday, October 29, 2011
Prevalence and Tracking of Back Pain From Childhood to Adolescence
It is generally acknowledged that back pain (BP) is a common condition already in childhood. However, the development until early adulthood is not well understood and, in particular, not the individual tracking pattern.
Prevalence of neck pain, mid-back pain and low back pain was tracked in children ages 9, 13 and 15.
The results were:
The prevalence estimates for children at the ages of 9, 13, and 15, respectively, were for Back Pain 33%, 28%, and 48%.
For Low Back Pain: 4% (9 y/o), 22% (13 y/o), and 36% (15 y/o).
For Mid Back Pain: 20% (9 y/o), 13% (13 y/o), and 35% (15 y/o)
Neck Pain 10% (9 y/o), 7% (13 y/o), and 15% (15 y/o).
Seeking care for Back Pain increased from 6% and 8% at the two youngest ages to 34% at the oldest.
What are the causes of back pain which were dismissed as "growing pains" years ago ? Numerous studies have reported: Back Pack use, texting, use of computers and lap tops and sporting injuries.
One of the main reasons that Chiropratic has become an ever increasing utilized service is it's drugless approach which is embraced by more and more parents and Pediatricians. Adolescents and teens typically have a very quick response and it is our hope that early spine care can stave off more serious spine problems in adulthood.
At Peninsula Spine & Sports Rehabilitation in San Mateo, Dr. Hindocha treats adolescents and teenagers with neck, mid-back and low back problems with gentle Chiropractic therapy including: therapeutic exercises and gentle soft tissue procedures. Dr. Hindocha's experience has been adolescents and teens respond very quickly to Chiropractic therapy. We are located in San Mateo, CA, and offer gentle Chiropractic therapy. Talk to your Pediatrician today !
Prevalence of neck pain, mid-back pain and low back pain was tracked in children ages 9, 13 and 15.
The results were:
The prevalence estimates for children at the ages of 9, 13, and 15, respectively, were for Back Pain 33%, 28%, and 48%.
For Low Back Pain: 4% (9 y/o), 22% (13 y/o), and 36% (15 y/o).
For Mid Back Pain: 20% (9 y/o), 13% (13 y/o), and 35% (15 y/o)
Neck Pain 10% (9 y/o), 7% (13 y/o), and 15% (15 y/o).
Seeking care for Back Pain increased from 6% and 8% at the two youngest ages to 34% at the oldest.
What are the causes of back pain which were dismissed as "growing pains" years ago ? Numerous studies have reported: Back Pack use, texting, use of computers and lap tops and sporting injuries.
One of the main reasons that Chiropratic has become an ever increasing utilized service is it's drugless approach which is embraced by more and more parents and Pediatricians. Adolescents and teens typically have a very quick response and it is our hope that early spine care can stave off more serious spine problems in adulthood.
At Peninsula Spine & Sports Rehabilitation in San Mateo, Dr. Hindocha treats adolescents and teenagers with neck, mid-back and low back problems with gentle Chiropractic therapy including: therapeutic exercises and gentle soft tissue procedures. Dr. Hindocha's experience has been adolescents and teens respond very quickly to Chiropractic therapy. We are located in San Mateo, CA, and offer gentle Chiropractic therapy. Talk to your Pediatrician today !
Does eating chocolate lower stroke risk ?
Chocolate lovers may have another reason to indulge. A new study shows that consuming chocolate on a regular basis may decrease stroke risk by 20%.
According to a recent study published in the October 18 issue of the Journal of the American College of Cardiology.
Chocolate is thought to have cardiovascular benefits resulting from the flavonoids in cocoa that have antioxidant properties. Antioxidants protect the body from damage caused by free radicals and can suppress oxidation of low-density lipoprotein. Dark chocolate consumption has also been shown to reduce blood pressure, which is a strong risk factor for stroke, as well as improve endothelial and platelet function and heighten insulin resistance.
Interestingly, women with hypertension had a reduction of stroke risk with chocolate consumption that was not statistically significant, whereas those without hypertension had a statistically significant risk reduction for stroke
According to a recent study published in the October 18 issue of the Journal of the American College of Cardiology.
Chocolate is thought to have cardiovascular benefits resulting from the flavonoids in cocoa that have antioxidant properties. Antioxidants protect the body from damage caused by free radicals and can suppress oxidation of low-density lipoprotein. Dark chocolate consumption has also been shown to reduce blood pressure, which is a strong risk factor for stroke, as well as improve endothelial and platelet function and heighten insulin resistance.
Interestingly, women with hypertension had a reduction of stroke risk with chocolate consumption that was not statistically significant, whereas those without hypertension had a statistically significant risk reduction for stroke
Alcohol & Sleep ?
Alcohol is often used by patients as a sleeping aid. Many patients say they have a drink to relax and help them sleep; yet those same patients often complain of sleep problems. Alcohol's effect on sleep has been extensively studied for more than 50 years. Certainly, it can help you get to sleep more quickly, but then its effect wears off and it can disrupt sleep.
They studied nearly 100 healthy adults; two thirds were women and one third were men. Participants were given either a placebo or an alcohol drink. Breath alcohol concentration was measured and those getting alcohol had to drink until intoxicated. They also filled out a questionnaire about sleep, both at bedtime and the following morning. Polysomnography was performed to monitor sleep patterns. The results showed that sleep quality ratings were worse for those drinking alcohol compared with those getting sham alcohol. There was also a sex difference. Women who had taken alcohol slept worse than the men who imbibed. The female drinkers had fewer hours of sleep and it was more disrupted. They woke more often and for longer periods. Researchers say the reasons could be explained by sex differences in alcohol metabolism.
They studied nearly 100 healthy adults; two thirds were women and one third were men. Participants were given either a placebo or an alcohol drink. Breath alcohol concentration was measured and those getting alcohol had to drink until intoxicated. They also filled out a questionnaire about sleep, both at bedtime and the following morning. Polysomnography was performed to monitor sleep patterns. The results showed that sleep quality ratings were worse for those drinking alcohol compared with those getting sham alcohol. There was also a sex difference. Women who had taken alcohol slept worse than the men who imbibed. The female drinkers had fewer hours of sleep and it was more disrupted. They woke more often and for longer periods. Researchers say the reasons could be explained by sex differences in alcohol metabolism.
Friday, October 28, 2011
Yoga, Stretching Ease Chronic Low Back Pain
An online study published on October 24 in Annals of Internal Medicine found that stretching, regardless of whether it is achieved via yoga classes or conventional stretching exercises, has moderate benefits in adults with moderately impairing chronic low back pain.
In a comparative effectiveness study, researchers found that yoga classes were more effective than a self-help book, but not more effective than stretching classes, in improving function and reducing symptoms resulting from chronic low back pain, with benefits lasting at least several months.
These results are encouraging and at Peninsula Spine & Sports Rehabilitation, I have encouraged my patients to take a more active role in managing their chronic low back pain.
If you suffer from Chronic Low Back Pain, we have had success in eliminating or greatly reducing symptoms and increasing our patients quality of life. We are located in San Mateo & San Francisco and we offer Chiropractic treatment with physiotherapy including core and cervical stabilization exercise programs and Spinal Decompression Therapy in San Mateo utilizing the VAX-D. Call us today for a consultation at (650) 347-2225.
In a comparative effectiveness study, researchers found that yoga classes were more effective than a self-help book, but not more effective than stretching classes, in improving function and reducing symptoms resulting from chronic low back pain, with benefits lasting at least several months.
These results are encouraging and at Peninsula Spine & Sports Rehabilitation, I have encouraged my patients to take a more active role in managing their chronic low back pain.
If you suffer from Chronic Low Back Pain, we have had success in eliminating or greatly reducing symptoms and increasing our patients quality of life. We are located in San Mateo & San Francisco and we offer Chiropractic treatment with physiotherapy including core and cervical stabilization exercise programs and Spinal Decompression Therapy in San Mateo utilizing the VAX-D. Call us today for a consultation at (650) 347-2225.
Thursday, October 27, 2011
Epidural Steroid Injections for Chronic Low Back Pain
An interesting study published in the British Medical Journal on the effects of Epidural Steroid Injections for Chronic Low Back Pain. Here are the highlights:
Epidural injections involve injection a steroid mixture into the Epidural space near the irritated nerve root. Participants received two injections with a two week interval.
A total of 116 participants were included in the study and they were split into 3 groups:
1.) Subcutaneous "sham" injections of 2 mL of 0.9% Saline solution (salt-water).
2.) Epidural injection of 30 mL of 0.9% Saline solution (salt-water).
3.) Epidural injection of 40 mg triamcinolone acetonide in 29 mL 0.9% saline.
Results:
All groups improved after the interventions, but we found no statistical or clinical differences between the groups over time.
At Peninsula Spine & Sports Rehabilitation, we offer a non-surgical treatment of chronic low back pain in San Mateo, CA. We offer VAX-D spinal decompression to treat chronic low back pain from: Sciatica, Herniated Discs, Degenerative Disc Disease, Spinal Arthritis. Please visit our Spinal Decompression website or schedule an appointment for your chronic low back pain treatment in San Mateo at (650) 347-2225.
Epidural injections involve injection a steroid mixture into the Epidural space near the irritated nerve root. Participants received two injections with a two week interval.
A total of 116 participants were included in the study and they were split into 3 groups:
1.) Subcutaneous "sham" injections of 2 mL of 0.9% Saline solution (salt-water).
2.) Epidural injection of 30 mL of 0.9% Saline solution (salt-water).
3.) Epidural injection of 40 mg triamcinolone acetonide in 29 mL 0.9% saline.
Results:
All groups improved after the interventions, but we found no statistical or clinical differences between the groups over time.
At Peninsula Spine & Sports Rehabilitation, we offer a non-surgical treatment of chronic low back pain in San Mateo, CA. We offer VAX-D spinal decompression to treat chronic low back pain from: Sciatica, Herniated Discs, Degenerative Disc Disease, Spinal Arthritis. Please visit our Spinal Decompression website or schedule an appointment for your chronic low back pain treatment in San Mateo at (650) 347-2225.
Consumer Reports rates Chiropractic for high patient satisfaction.
Buying a new car ? TV ? Digital camera ? Where do we turn to ? The choice is clear, most people will research their next big purchase on the internet. There are many great review sites available such as Yelp, CNET and of course Consumer Reports.
Consumer reports conducted an online survey of more than 45,000 of their subscribers on Alternative Health Care usage. Here are some of the highlights:
Back Pain: 36% of survey respondents utilized chiropractic for back pain; 65% said it "helped a lot." Compare that with 38% of respondents who utilized prescription medications; 53% said it "helped a lot". 58% of respondents utilized over-the-counter medication with 28% stating "substantial relief".
Neck Pain: 41% of survey respondents utilized chiropractic for neck pain; 64% said it "helped a lot." Over-the-counter and prescription medications were the second and fourth most utilized treatment methods (56% and 33%), but only 39% (over-the-counter) and 25% (prescription), respectively, said the medication "helped a lot."
With statistics like these, should Chiropractic still be considered "alternative" treatments or is it time this becomes the first line of spine care ?
Consumer reports conducted an online survey of more than 45,000 of their subscribers on Alternative Health Care usage. Here are some of the highlights:
Back Pain: 36% of survey respondents utilized chiropractic for back pain; 65% said it "helped a lot." Compare that with 38% of respondents who utilized prescription medications; 53% said it "helped a lot". 58% of respondents utilized over-the-counter medication with 28% stating "substantial relief".
Neck Pain: 41% of survey respondents utilized chiropractic for neck pain; 64% said it "helped a lot." Over-the-counter and prescription medications were the second and fourth most utilized treatment methods (56% and 33%), but only 39% (over-the-counter) and 25% (prescription), respectively, said the medication "helped a lot."
With statistics like these, should Chiropractic still be considered "alternative" treatments or is it time this becomes the first line of spine care ?
Wednesday, October 26, 2011
Diagnosis - Arthritis
Definition:
Arthritis is a general term referring to a joint disorder affecting one or more joints. There are over 100 different types of Arthritis including: Degenerative Joint Disease, Rheumatoid Arthritis, Gout, Psoriatic Arthritis, Stills disease, Ankylosing Spondylitis, etc.
Classification:
Arthritis can be classified as: inflammatory (Rheumatoid), degenerative (Osteoarthritis) or metabolic (Gout).
Causes:
The most common form of Arthritis is Degenerative Joint Disease (also known as Osteoarthritis, Spondylosis, Osteoarthrosis, Degenerative Osteoarthritis, Degenerative Osteoarthrosis).
Degenerative Joint Disease is the more accurate term, replacing Osteoarthritis, as Osteoarthritis indicates that it is an inflammatory arthritis which is incorrect.
Arthritis can be primary or secondary. Primary Osteoarthritis is idiopathic (no known cause). It is widely thought that this is caused by abnormal stresses on the joints which erodes the cartilage in a non-uniform fashion or normal stresses acting on "weakened" joints. Although aging does not cause arthritis, there is an association. Secondary Osteoarthritis results from chronic or sudden injuries to the joints such as: trauma, sporting injuries, repetitive stress injuries, poor posture, certain metabolic disorders (Gout) and many other factors.
Symptoms:
Degenerative joint disease can affect weight bearing joints such as: knees, hips, spine as well as other joints such as: hands, fingers, shoulders and fingers.
Symptoms include: morning stiffness - due to the joints being relatively immobile at night, pain - due to cartilage erosion, less fluid in the joint space, "bone-on-bone" contact, less flexibility - due to cartilage erosion and "popping and crackling" of the joints - due to uneven cartilage erosion.
Diagnosis:
A thorough history and physical exam can help distinguish between primary and secondary arthritis. However, X-ray, MRI or CT scan will provide a definitive diagnosis.
Treatment:
Medical treatment involves the use of medication called NSAID's (non-steroidal anti-inflammatories). There has been some concern in the recent years due to long term use of these medications which have been linked to: ulcers, liver and kidney failure and cardiovascular events (heart attacks). Since Arthritis is a chronic disease, unfortunately, lifetime medication usage is the primary mode of treatment.
Chiropractic treatment focuses on spinal manipulation of the involved joints. Careful manipulation of the involved joints can decrease pain and restore motion.
Generally, many patients benefit from light exercises and the self-application of heat.
At Peninsula Spine & Sports Rehabilitation, we offer a non-surgical, non-pharmacological, treatment and rehabilitation of degenerative joint disease and degenerative disc disease. Please call us today at (650) 347-2225 for an initial consultation.
Arthritis is a general term referring to a joint disorder affecting one or more joints. There are over 100 different types of Arthritis including: Degenerative Joint Disease, Rheumatoid Arthritis, Gout, Psoriatic Arthritis, Stills disease, Ankylosing Spondylitis, etc.
Classification:
Arthritis can be classified as: inflammatory (Rheumatoid), degenerative (Osteoarthritis) or metabolic (Gout).
Causes:
The most common form of Arthritis is Degenerative Joint Disease (also known as Osteoarthritis, Spondylosis, Osteoarthrosis, Degenerative Osteoarthritis, Degenerative Osteoarthrosis).
Degenerative Joint Disease is the more accurate term, replacing Osteoarthritis, as Osteoarthritis indicates that it is an inflammatory arthritis which is incorrect.
Arthritis can be primary or secondary. Primary Osteoarthritis is idiopathic (no known cause). It is widely thought that this is caused by abnormal stresses on the joints which erodes the cartilage in a non-uniform fashion or normal stresses acting on "weakened" joints. Although aging does not cause arthritis, there is an association. Secondary Osteoarthritis results from chronic or sudden injuries to the joints such as: trauma, sporting injuries, repetitive stress injuries, poor posture, certain metabolic disorders (Gout) and many other factors.
Symptoms:
Degenerative joint disease can affect weight bearing joints such as: knees, hips, spine as well as other joints such as: hands, fingers, shoulders and fingers.
Symptoms include: morning stiffness - due to the joints being relatively immobile at night, pain - due to cartilage erosion, less fluid in the joint space, "bone-on-bone" contact, less flexibility - due to cartilage erosion and "popping and crackling" of the joints - due to uneven cartilage erosion.
Diagnosis:
A thorough history and physical exam can help distinguish between primary and secondary arthritis. However, X-ray, MRI or CT scan will provide a definitive diagnosis.
Treatment:
Medical treatment involves the use of medication called NSAID's (non-steroidal anti-inflammatories). There has been some concern in the recent years due to long term use of these medications which have been linked to: ulcers, liver and kidney failure and cardiovascular events (heart attacks). Since Arthritis is a chronic disease, unfortunately, lifetime medication usage is the primary mode of treatment.
Chiropractic treatment focuses on spinal manipulation of the involved joints. Careful manipulation of the involved joints can decrease pain and restore motion.
Generally, many patients benefit from light exercises and the self-application of heat.
At Peninsula Spine & Sports Rehabilitation, we offer a non-surgical, non-pharmacological, treatment and rehabilitation of degenerative joint disease and degenerative disc disease. Please call us today at (650) 347-2225 for an initial consultation.
Subscribe to:
Posts (Atom)